why endometriosis is a feminist issue
In issue 118, Angie Mashford-Scott writes about her struggles dealing with endometriosis.
I would bet my favourite heat pack and all the gin in my pantry that if you asked anyone with endometriosis if they’ve had their symptoms dismissed by a medical professional, have gone a long period of time with no diagnosis or a misdiagnosis, and have been made to feel like they’re exaggerating or have a low pain threshold, they would say, “Yes.”
It’s no wonder the medical community has such a poor understanding of women’s bodies and the illnesses that predominantly affect us. Throughout history, doctors have minimised women’s pain and dismissed symptoms as having a psychological origin. In other words, “it’s all in their heads.” This has deep roots in what the Ancient Greeks called “hysteria”.
Hysteria was believed to be a medical condition specific to women and caused by problems of the uterus. Symptoms included anxiety, being “excessively emotional”, and various physical symptoms including pain. Plato famously stated that when women deny their “biological destiny” to reproduce, their uterus becomes “suffocated”, sad and angry, and this causes physical and mental illness. (Fun fact: the word hysteria derives from the Greek word “hystera”, meaning uterus.)
Oh but it gets better. During the Middle Ages, hysteria was attributed to a woman and her uterus being possessed by evil spirits and the devil. Then in Renaissance times, it was believed that hysteria was actually sexual in nature and potentially due to a problem with the woman’s genitals or promiscuity.
By the 19th century, we had moved from seeing hysteria as just a physical problem to a psychological problem (thanks, Freud!). A woman who kept returning to the doctor, voiced ongoing concerns or “failed” to respond to treatment was seen as difficult and unstable. If a doctor couldn’t find a physical cause for a woman’s symptoms and suffering, she would be told that there was nothing physically wrong and her mind was likely overstimulated (for which, of course, she had limited capacity). Or, if she was particularly unlucky, she would be institutionalised and subjected to a range of obscene treatments.
Advances in science and surgical techniques during the 20th century helped develop our understanding of many diseases, including endometriosis. However, hysteria’s legacy lived on. Societal attitudes and misogyny ensured that the burden of blame remained on women themselves, myths were still widespread, and women’s own reports were not viewed as reliable. Pelvic and menstrual pain continued to be associated with sexually transmitted pelvic inflammatory disease, promiscuity and mental illness, or was normalised as “women’s troubles”.
In the late 20th century, endometriosis got the fun nickname “the career woman’s disease”. It was widely believed to be a disease that mostly affected women in their 30s who had careers and delayed having children – the cruel irony being that endometriosis is the leading cause of fertility challenges in women. Which meant that some women, desperate to have children but unable to become pregnant, were stigmatised and judged for not prioritising motherhood.
So let’s recap. Over the past 2000 years, women’s mental and physical health problems have been attributed to having an angry, empty uterus, being possessed by evil spirits, sexual deviance, the overstimulation of our inferior minds, and selfishly delaying motherhood. I mean, what a complete clusterfuck of fuckery.
No wonder women today still battle against a stigma and stereotype that we're sensitive hypochondriacs and our accounts of our own pain and symptoms are unreliable. This, paired with society’s undervaluing and underinvesting in women’s medical research, means that there is still no known cause or cure for endometriosis. Current treatments are largely ineffective, and on average, a woman will see eight doctors over seven to 10 years before she even receives a diagnosis.
This experience of having your symptoms brushed off or normalised (“some women just have these troubles”) is so common that many endo patients (me included) are known to tearfully express relief and gratitude when they wake up from surgery and hear that the surgeon did indeed find endometriosis. In a 2015 Guardian article, Gabrielle Jackson wrote about feeling vindicated when her surgeon showed her pictures and said, “Look how bad it was.” She wrote, “Now I had a disease with a name and I didn’t have to feel like I was making it up any more.”
The systematic minimising and gaslighting of women’s pain and experiences leads us to lose trust in our own perception and judgement, and to actually start gaslighting ourselves. You wonder, “Maybe I am just not able to cope as well as others. Maybe I am being dramatic. Maybe it isn’t that bad.” And this can have devastating consequences.
Following my most recent laparoscopic surgery, I was rushed back into hospital and admitted to the intensive care unit with life-threatening sepsis. Like many endo patients, I had questioned the severity of my deteriorating condition and delayed going back into hospital, which almost cost me my life.
I was in severe pain. I was nauseous and vomiting. I couldn’t eat or drink. I was groaning and crying. When I called the hospital to report how bad my pain and condition was, the nurse said, “Well you have just had surgery, dear. Have you taken all of your pain medication?” I hadn’t because I couldn’t even keep water down. But I still thought to myself, “Maybe the problem is that I haven’t taken all my medications.” So the delay stretched on until I couldn’t take it anymore.
When the paramedics arrived, I could see by the look in their eyes and swiftness of their actions that they saw what I felt. This was now a medical emergency. My system was shutting down.
I didn’t want to be dramatic. I didn’t want to waste anyone’s time. Didn’t want to present at the emergency department just to be told that what I was experiencing was “normal” surgery recovery. Even though I knew deep down it wasn’t, I didn’t have the strength of conviction. Hysteria’s legacy had planted the seeds of self-doubt into my DNA. And my experiences with the medical system had helped them flourish.
Endometriosis is more than a physical illness. It’s a social, political and economic one. Sexism and gender bias has determined what we know about women’s health and biology, what research is funded, and the quality of medical care and treatment that we receive.
Gender-diverse individuals with endometriosis can have even greater challenges to their care, often not meeting the set criteria to receive care and treatment within current medical and social systems. Additionally, they are often excluded from women's health narratives around the disease, effectively erasing their experiences from the discussion.
It is now believed that many historical descriptions of hysteria were most likely undiagnosed cases of endometriosis. Society needs to woman the fuck up and turn this ship around. It’s gone on long enough.
See more from Angie over here.
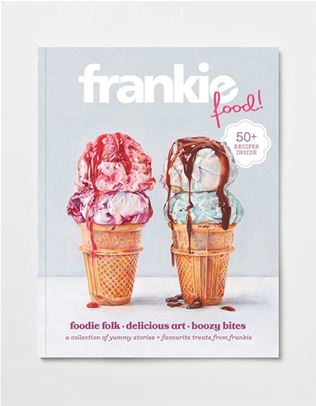
This article comes straight from the pages of issue 118. To get your mitts on a copy, swing past the frankie shop, subscribe or visit one of our lovely stockists.









.jpg&q=80&w=316&c=1&s=1)


.jpg&q=80&w=316&c=1&s=1)